The cure for colic
When Oliver James's newborn son got colic, he and his wife prepared
themselves for the horror of sleepless nights. Then they attended a
breastfeeding clinic ...
Two weeks after our son Louis was born, three months ago, he started
showing signs of colic. Just when my wife Clare and I were at our most
exhausted, at around six in the evening, he would cry loudly and
inconsolably for no apparent reason, his back arched and his legs
doubled up. Since our daughter Olive (now three) had done the same, we
were not altogether surprised. But we groaned at the prospect of months
of long nights walking him around to no avail and nocturnal drives with
the Pet Shop Boys Introspective album blaring. (This was the only thing
guaranteed to shut our daughter up. Somebody should do a study of which
popular music is most effective in quieting troubled babies - I swear by
the Pets.)
To add to the grief, my wife got mastitis, which we assumed was the
reason each feed felt as if she were having her nipples slashed with
razor blades. The antibiotics to treat it only made our son worse,
upsetting his tummy. As we lurched towards meltdown and bottle-feeding, a
health visitor suggested we visit midwives Chloe Fisher and Sally Inch,
said to be the international queens of breastfeeding, at their drop-in
clinic at Oxford's John Radcliffe Hospital.
That they could help us with the mastitis seemed plausible,
but I was sceptical when Fisher told us that the colic was also to do
with my wife's breastfeeding technique. I had studied the scientific
literature in the past, and despite contact with dozens of health
professionals over the years, and endless discussions with other
parents, no one had told us that colic had anything to do with how you
breastfeed.
About one-fifth of all babies get the full colic syndrome, of whom
only a small minority (5-10%) have any identifiable physical cause. It's
a serious problem because half of those mothers with severely colicky
babies are liable to become mentally ill, falling to one-quarter if the
baby is only moderately colicky (compared with 3% of mothers with none).
The
ailment has baffled medical scientists seeking a biological cause. Only
social, rather than medical, science seems to provide some clues. Most,
if not all, babies in developed nations get some of the symptoms, yet
it is rare or unknown in developing ones. A possible reason is that in
the latter countries, babies are constantly held, fed effectively and on
demand. Babies cry less whose mothers carry them for three hours or
more, or feed on demand during the first two months.
Another reason could be the lack of social support and the
hard-working, stressful lives of pregnant mothers in developed nations. A
study of 1,200 mothers interviewed prenatally and when the child was
three months found that a good relationship with the partner before the
birth reduced colic. Seventy per cent of mothers had colicky babies if
they had a lot of prenatal stress, felt isolated and anticipated needing
a lot of postnatal help, compared with only 25% of babies of mothers
without these problems. Prior problems with the mother's mother also
predicted it. When asked during pregnancy or shortly after the birth,
mothers who recalled distressing childhood memories or expected a lack
of support or excessive interference from their mothers were more likely
to have a colicky baby.
It came, therefore, as a great surprise to me when Fisher told us
that colic in the breastfed baby is primarily due to something as simple
as not attaching the baby to the breast correctly, which means that the
baby is unable to "drain" the breast properly during feeds.
Arriving at the clinic on a Monday afternoon, we were met by the
sight of a clutch of desperate mothers, their babies suckling for
Britain. There were two pairs of twins; our frazzled minds boggled at
the prospect of trying to keep them satisfied. But Fisher and Inch
radiated supreme confidence that salvation was at hand, roving round the
room, providing emphatic instructions.
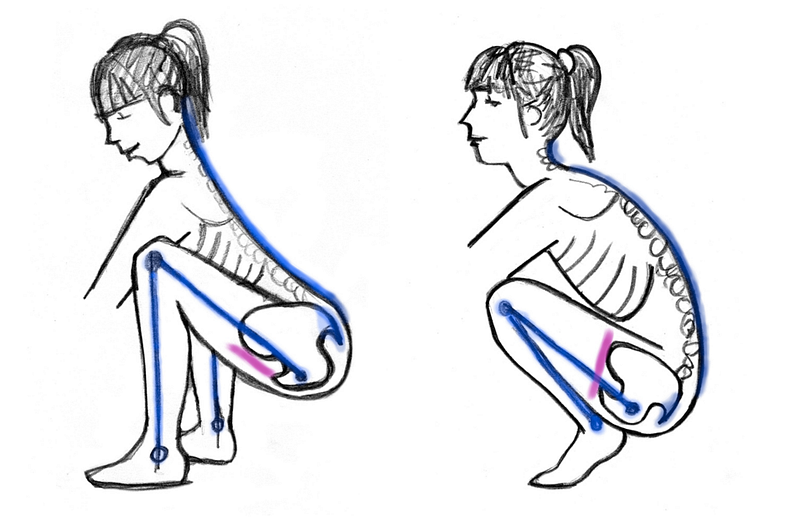
Fisher
enunciated two principles: "First, don't assume the breast is like a
bottle. The milk is in the breast, not in the nipple, whereas with a
bottle, the milk is in the teat. To feed effectively from the breast the
baby must scoop in a deep mouthful of breast, whereas with a bottle, it
can just suck on the end of the teat.
"Second, people wrongly assume the middle of the baby's mouth is
halfway between the top and bottom lip. In fact, the middle is between
the upper surface of the tongue and the upper palate. For the baby to
draw sufficient breast tissue into its mouth, it must be able to get its
tongue well away from the base of the nipple and that won't happen
unless the breast is presented between the tongue and the upper palate."
If the baby did not attach properly, the midwives told us, it would
not drain the breast properly and would keep compressing the nipple
between the tongue and hard palate, turning it into something resembling
minced lamb. Putting this into practice proved surprisingly difficult
but after a bit my wife got the hang of it.
Next came the other important point: "Only switch breasts when the
well-attached baby comes off the breast spontaneously and seems
completely satisfied," said Fisher. "In offering the second breast, let
the baby decide whether he wants it. If the mother starts each feed on
alternate breasts [regardless of whether the baby has had one or two at a
feed], the breasts will get roughly even use. The important thing is to
allow the baby to finish the first breast first."
Failing to do this is the main cause of colic. Fisher also told us
that the initial milk is low in fat and calories. If you switch breasts
before the high-fat milk has been drunk, the baby will take more from
the second breast than he would otherwise have done. Despite the
relatively huge volume of liquid in its stomach, the baby will then be
wanting another feed before long, because low-fat feeds are processed
quickly, leading to a pattern of very frequent feeding. This can cause
mental illness-inducing sleep-deprivation, but worst of all, it will
cause colic.
Both poor attachment and breast switching result in the baby taking
frequent, large-volume, low-fat feeds, which in turn lead to rapid
emptying of the stomach into the large intestine. If too much gets there
too fast, there is not enough of the enzyme lactase to break the sugar
in the milk (lactose) down. The gut turns into a malfunctioning brewery,
with fermentation of the sugar in the excess milk creating gas and
explosive poos. The crying, arched back, rigid tummy and irritability of
colic follow.
I was flabbergasted. If all this were really true, why on earth
wasn't everyone told about it, especially considering the damage done to
the mental health of parents by colic? Fisher replied that she and Dr
Mike Woolridge had published the hypothesis in the leading medical
journal the Lancet 17 years ago. "I was expecting that after that it
would solve the problem. It seems pretty extraordinary to me that it has
not."
Fisher believes she is right because she has seen thousands of
mothers solve the problem by following their advice, but since the 1988
paper, her theory has been scientifically tested. A 1995 study compared
two groups of 150 mothers: one asked to let the baby terminate the feed
on the first breast; the other asked for the baby to feed equally from
both breasts. Twice as many of the mothers who fed equally with both
breasts had colicky babies (23% versus 12%). What is more, finishing the
first breast first resulted in significantly less breast engorgement.
This turned out to apply to us too. Inch doubted that my wife
actually had infectious mastitis or had needed antibiotics for it and
easily proved her point. A few days after my wife had started taking the
antibiotics, the problem had developed in the right as well as the left
breast. Since infectious mastitis is a bacterial problem, and since the
germs should have been killed by the antibiotics, Inch pointed out that
such a transfer could not have happened if it was a bacterial
pathology. Rather, the inflamed breast was due to back pressure within
the ductal system of the breast, she said. Ineffective milk removal was
not keeping pace with milk production so the milk could no longer be
contained within the ductal system. It was forced into the connective
tissue of the breast, where it gets treated as a foreign protein, with
subsequent inflammation and pain.
All
of which proved to be of more than academic interest to us. While we
returned to the Thursday clinic for a booster course in attaching to the
breast, from the first moment my wife did it properly, the pain was
much less. From that very night our son was free of colic and within a
week, the "mastitis" was disappearing.
This is very good news for women suffering the curse of colic who are dedicated breast feeders. I always thought breastfed babies could not get colic. Will pass thin info on to all my new mums.






 I can't believe how quick it all was!
I can't believe how quick it all was!