The forgotten art of untucking the tail.
This post was originally published on 7 Nov 2015 at www.yogawithivana.com
A tiny detail we’ve lost since the hunter-gatherer times and how to fix it
I’ve
been spending most of my time lately learning about biomechanics,
healthy alignment and how movement affects our bodies in relation to
gravity. The research from the last few years shows that the way we move
affect us not only mechanically, as it was previously thought, but also
causing biochemical changes on cellular level, changing us from inside
out. This process of the body adapting to and being shaped by movement
is called mechanotransduction.
We seem to be living in the world that encourages sitting with the tail tucked under.
The
furniture we use sitting all day is optimised for comfort and
convenience, but usually not ergonomically adapted for pelvic floor
health. Who would even think about that?
There
is a well spread myth in our society that pelvic floor issues are a
normal consequence of pregnancy and birth, or ageing for men. But we
would rarely think of looking for a cause a bit deeper, in the way we
have been living and moving before that.
Did
you know that the anatomic function of our remnant of a tail is,
amongst others, to control opening and closing of the pelvic outlet. If
you look at a dog, or a another tailed animal, you can see that they
keep their tail up, happily wagging when they are in a good mood. And
this is the default. When you see a dog wearing his tail down between
his back legs, it is usually a sign that the dog is on the fight of
flight mode and his pelvic floor is tense as a part of his whole body
reacting to danger.
Even
though we now have only the beginning of what was once a real mammalian
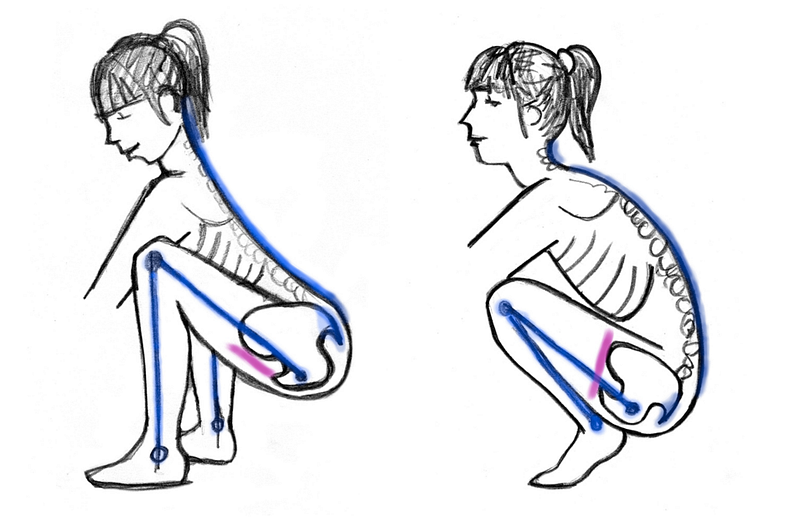
tail, it behaves the same. Untucking the tailbone opens the pelvic
outlet, tucking it closes it — tightening the pelvic floor. The dog with
his tail down between his legs is an equivalent of you sitting on your
sacrum, the back supported by a chair or a couch. If you spend multiple
hours a day in this position, your pelvic floor doesn’t really have a
chance to release and allow the muscle fibres to regain their natural
length at resting state. So gradually it shortens.
In his book Pelvic Power, Eric Franklin
compares natural movement of the pelvic floor to a kite. As you stand
up the pelvic floor slightly lifts and narrows similarly to a kite
picking the wind and taking off. Reversely, as you sit down (with
untucked tail, using your sitbones) the pelvic floor widens and releases
to its full length, like a kite descending down, opening and landing.
But what if we never allow it to release?
Tight muscle does NOT equal a strong muscle.
Biomechanicist Katy Bowman
compares an optimally functioning pelvic floor to a trampoline. It
supports the weight of all our pelvic organs and allows any extra load
to just bounce off its healthy, elastic fibres, tensing and releasing
naturally. Keeping the muscles short all the time doesn’t let them
perform their function optimally. And further on, as our bodies
naturally adapt to the way we use them, we gradually end up with
shortened muscles.
This
is further exacerbated by using pelvic floor exercises (‘Kegels’) on
‘the more the better’ basis — Bowman explains. Doing more and more
repetitions of contractions of the muscle isolated from the rest of the
body without allowing it to ever fully release, you get a muscle that is
tight and locked short. Tight muscle does NOT equal a strong muscle. A
strong muscle is able to both fully contract and fully release.
So why I am telling you all this now? Reading Katy Bowman’s last book — Move Your DNA,
I’ve started to incorporate more movement into my life other than and
independently from exercising. And especially, I’ve started to squat more, when playing with my toddler, picking things off the floor and even going to the toilet.
Learning
to untuck my tail has made me finally realise why I still had to push
my baby out and not bear it gently down, letting the gravity do the job,
in spite of all the birth preparations and beautiful relaxation
techniques I mastered beforehand.
To “breathe the baby out” you have to first untuck your tail.
Anatomically,
in order for the baby to come out the pelvic floor has to release, but
you can’t possibly release the pelvic floor with the tailbone tucked
under. You can only use the strength of your muscles (transverse
abdominals and diaphragm as they instruct you to hold your breath and
“puuuuussssh!”) against your pelvic floor. And that’s a sure way to end
up with a nice tear and possibly a pelvic floor disfunction. I was lucky
that the athletic challenge, how my birth experience felt to be honest,
ended without any serious damage. My body just took over at the last
moment and following a very primal instinct jumped on a dining chair
opening the pelvic outlet fully. The squats and kneeling with rounded
back would have probably taken me to an assisted delivery.
“Modern
birthing science has placed a large burden on secreted hormones (like
relaxin) to prepare the body for needed mobility.” Katy Bowman says.
Yes, hormon relaxine is useful in letting the body open up for the
birth, but it’s not enough, unless we have strong muscles that can fully
contract, but also fully release. But then, strong isolated muscles are
not enough either. In order to have smooth births we ned to have a
whole-body endurance. A great way to develop endurance is to walk as
much as you can. “The woman who wants to go about a birthing process
naturally can follow the lead other “natural” processes women have been
doing for millennia — walking 5–6 total miles per day, and squatting to
bathroom multiple times daily.” — she adds.
So,
the bottom line is: get off your tail and sit on your sit bones
instead, walk more, squat more, move more. It’s all about really using
the body. Reintroducing a variety of movement we can strengthen the
muscles of the pelvic girdle and release our tail once again, allowing
it to respond freely to the demands of natural movement. And this can
make a big difference for our pelvic floor health and the general level
of our wellbeing.
Even more reason to keep off the bed during labour and birth? Not sure about "squatting to bathroom" though, sounds messy.
 I can't believe how quick it all was!
I can't believe how quick it all was!

